This story is part of a partnership with ProPublica and reporters Maya Miller and Robin Fields.
Scripps News and ProPublica engaged in a joint investigation this past November that focused on insurance companies rejecting millions of treatments in this country.
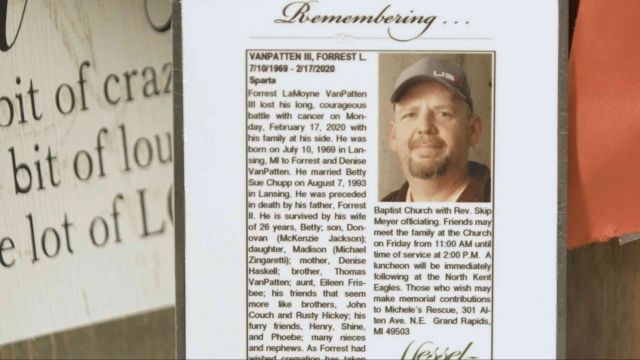
Our report examined the case of Forrest VanPatten, a Michigan man who died in 2020 after his insurance company denied coverage of his cancer treatment, despite a state law requiring cancer drugs be covered.
Now, two months after our investigation was broadcast, state regulators in Michigan are putting insurers on notice.
The state of Michigan this week sent an official bulletin to insurers stating that genetic therapies to treat cancer must be covered.
Sadly, that definitive message came too late for the VanPatten family, who we met in Michigan at their family home late last year.
Memories of Forrest, their larger-than-life father and husband, are still raw nearly four years after he passed away.
“Just the unfairness of it. I guess it felt like it just got ripped away from us so quickly. So, so young,” said Betty VanPatten, Forrest’s wife of 26 years.
He died after a long battle with an aggressive form of lymphoma. He was just 50 years old.
“When he walked in a room, you knew it,” Betty told us. “He was just the light. He was my one.”
She told us that light went out just days after their insurance company denied coverage of a clinically proven treatment — a treatment that doctors believed was his last chance to extend his life.
“They took all his hope away,” Betty said. “There was always hope. There was always tomorrow. And when they denied it, that was the worst possible thing they could have done to him.”
In a heartbreaking interview with our Scripps News Grand Rapids station before he died, Forrest VanPatten said he felt like his insurance company was casting him aside.
“I feel like I'm being ignored, left out to die,” he said.
His medical team had just made one final plea to try to get his insurer to overturn its decision, but Forrest said he had become accustomed to the same response.
“Everything that gets processed through the insurance company is just a rejection of rejection. Rejection,” he said. “We need to push and push and push because there's nothing else.”
SEE MORE: How an insurer abandoned a cancer patient in his most critical hour
Forrest VanPatten died days after his interview not knowing Michigan had long required health insurers to cover cancer drugs, by law.
Our Scripps News investigation with ProPublica revealed that VanPatten’s insurer, Priority Health, came up with a semantic workaround to justify denying him coverage, by calling the costly treatment a gene therapy instead of a cancer drug. Executives claimed they had no obligation to cover gene therapies under state law.
Now, nearly four years after VanPatten’s death, the state of Michigan issued an official notice telling insurance companies that, by law, they cannot deny coverage for clinically proven treatments.
In a press release announcing the action, the director of Michigan’s Department of Insurance and Financial Services said, “to help ensure that life-saving cancer treatments are accessible and affordable ... health insurers … may not exclude coverage for cancer therapies, including genetic therapies or immunotherapies.”
VanPatten’s insurer, Priority Health, told Scripps News that they eventually began covering the therapy Forrest VanPatten needed after clinical work improved the treatment. A spokesman wrote to Scripps News this week: “We follow all state and federal coverage requirements ... We welcome the opportunity to answer any questions from legislators about coverage decisions.”
Forrest VanPatten’s wife Betty VanPatten told us knowing that the state of Michigan was finally taking action moved her to tears.
She said she was grateful that something positive was coming from her husband’s agonizing ordeal because she doesn’t want any other family to go through what hers did.
Trending stories at Scrippsnews.com